18 November 2014
Pregnant women with HIV can take three anti-HIV medicines instead of one to reduce the risk of their infants contracting the virus, according to results of a study released yesterday.
Before medicines to treat HIV became available, pregnant women with the virus had about a 40% risk of transmitting it to their newborn infants. Most of these infections took place during labour, but a significant minority occurred during breastfeeding. With the advent of anti-HIV medicines, called antiretrovirals, the risk of transmission came down dramatically.
In the early 2000s, it was vociferously debated whether HIV-positive women should breastfeed or use formula milk. Breastmilk is better for babies than formula milk, but with it comes the risk of HIV infection. Research results gave contradictory answers depending on many variables.
But in recent years the debate subsided because it was found that by giving HIV-positive mothers antiretroviral medicines, they could reduce the risk of the virus transmitting during breastfeeding to a very low rate.
Today in South Africa, fewer than 3% of children born to HIV-positive women are infected by a few weeks after birth, though the percentage likely becomes higher by the end of the breastfeeding period.
However, there are several research questions that need to be answered to reduce infection rates even further. For example:
Also, what options are best for the health of HIV-positive women, not only their infants?
Early results of the PROMISE study released yesterday take a step toward answering these questions. The study is looking at how different antiretroviral strategies can safely reduce the risk of HIV transmission from mothers to their babies. It is also examining the effect of two antiretroviral strategies on the health of women after they stop breastfeeding.
Over 3,500 HIV-positive pregnant (or recently pregnant) women are participating in the trial from India, Malawi, South Africa, Tanzania, Uganda, Zambia and Zimbabwe. None of them had yet progressed to AIDS when they enrolled in the trial. This means that on average they were much healthier than the general pregnant HIV-positive population. The trial’s main sponsor is the United States National Institutes of Health (NIH).
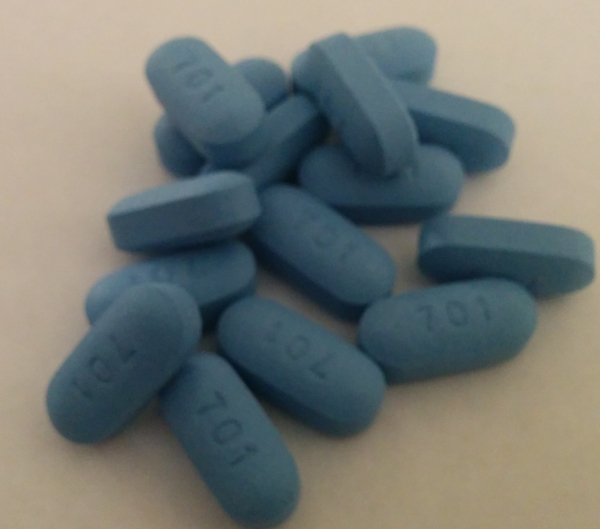
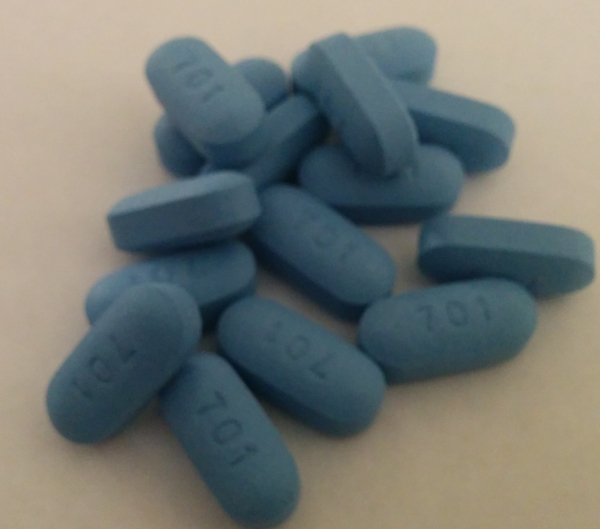
In a press release, the NIH said that an analysis of the study results until now has shown that by women taking three antiretrovirals instead of one from 14 weeks of pregnancy, they reduced the risk of HIV transmission to their babies. The babies were tested when they were two weeks old. Both strategies have been known to be effective, but it was not known if the triple-drug regimen would be better. Overall though, transmission throughout the trial has been low; only 1.8% in babies whose mothers took the single-drug regimen versus about half-a-percent in those whose mothers took triple-drug regimens.
Polly Clayden, an activist who edits HIV Treatment Bulletin South told GroundUp that the number of HIV infections was very low. “It will require programmatic work to reproduce these controlled trial results across sub-Saharan Africa,” she said. She also said the results confirm what’s currently recommended in South African and World Health Organisation guidelines.
Professor James McIntyre is the vice-chair of the IMPAACT Network, the organisation running the trial. He said, “We now have a randomised trial showing that triple-drug antiretroviral treatment is incredibly effective at preventing transmission of HIV.” But he cautioned, “Remember though this is only 14 days [when the babies were tested].” He said there would be further follow-up but that the half-a-percent transmission rate was remarkable.
McIntyre also said that there were more adverse pregnancy outcomes in the women who took three drugs, particularly early delivery, but he said, “These have not occurred at a high enough rate to worry. The team is still looking at all the details of this. I think the triple-drug therapy arm is doing better [when the fewer infections that result from triple-drug therapy are compared to the higher number of adverse pregnancy outcomes it causes]. By the end of the trial we’ll be able to give a thorough analysis.”
The study has also found that taking a regimen containing the antiretroviral drugs AZT, lamivudine and lopinavir resulted in fewer severe adverse pregnancies than a regimen containing the drugs tenofovir, FTC and lopinavir. This was an unexpected result, as tenofovir and FTC have usually proved to be better drugs than AZT and lamivudine in clinical trials in other HIV-positive populations.
McIntrye said, “We don’t yet know why [the tenofovir/FTC] arm had more adverse events. We’re investigating this, particularly whether this is because of [drug interactions with lopinavir and another drug called ritonavir]. But we don’t know enough about the effects between these two regimens to make a recommendation one way or another.”
The trial is continuing because, as Clayden explains, “PROMISE will also look at whether it’s better for the women to continue treatment after they’ve finished breastfeeding or not.” The trial will also hopefully answer which antiretroviral strategy is best for reducing transmission during breastfeeding.