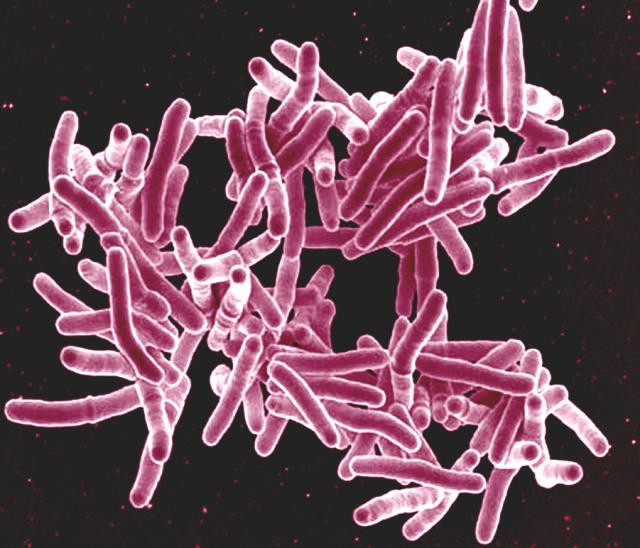
Electron micrograph of Mycobacterium tuberculosis bacteria, the cause of TB. Photo: NIAID via Flickr (CC BY 2.0)
10 July 2019
It is crucial to monitor patients taking the new drug for multidrug-resistant tuberculosis (MDR-TB), bedaquiline, to prevent resistance.
A study showed that resistance to bedaquiline emerged, despite a patient adhering to the standard treatment regimen, which requires bedaquiline to be taken along with at least five antibiotic drugs.
Scientists from Stellenbosch University (SU), the University of Cape Town (UCT) and international colleagues published their finding in the New England Journal of Medicine. They studied a 65-year-old, HIV-negative man, who was diagnosed with MDR-TB.
Despite the treatment he developed resistance to bedaquiline two months into treatment.
Bedaquiline is a promising new drug to treat a disease that has seen very few new treatments over the past few decades. The problem with the older drugs is that many patients are contracting strains of TB that are resistant to them.
New drugs are needed for which there are currently no — or very few — resistant strains of TB about. Usually doctors expect resistance to develop in a patient when their adherence is poor (i.e. they don’t take the medicine as prescribed), but this study suggests that resistance to bedaquiline can occur even in adherent patients.
Prof Helen Cox from the Institute of Infectious Disease and Molecular Medicine at UCT, said they did not “expect resistance to bedaquiline to emerge when the patient was receiving what we expected would be an effective multi-drug treatment regimen. We always treat TB with multiple antibiotics in case resistance to one of the drugs being used develops.”
In July last year, South Africa rolled out bedaquiline in its national programme. According to the World Health Organisation over 3% of new TB cases across the world are MDR-TB. It was estimated that in 2017 about 14,000 patients in South Africa had MDR-TB.
Dr Margaretha de Vos, from the Division of Molecular Biology and Human Genetics at Stellenbosch University and her colleagues Prof Rob Warren and Dr Serej Ley studied the development of resistance in the patient using a new techniques. They explained to GroundUp how it was done:
The entire DNA (the genome) of the TB bacteria was taken from samples of the patient’s sputum (phlegm) and then deciphered. Actually several samples were taken throughout treatment and from each of these samples the TB DNA was sequenced.
The different samples were compared to each other. The researchers identified changes (mutations) that arose in the DNA over time, while the patient was on treatment. Some of these mutations can cause resistance against the treatment. This is a very useful tool to identify new mutations that can cause drug resistance.
Only the bit that is known to cause resistance to bedaquiline was sequenced. Because only a small bit was sequenced, the scientists could sequence more DNA molecules at a time.
The TB bacterium only has one chromosome and so in effect one DNA molecule represents one TB bacterium. The number of bacteria in a patient can vary from thousands to millions. It only takes one bacteria to acquire the mutation that causes drug resistance for resistance to spread.
When that happens, this particular bacterium has an advantage over other bacteria that don’t have the mutation. The ones that do not have the mutation will be killed by bedaquiline while the bacteria with the mutation will multiple and eventually be the only “type” left in the whole population.
This process however takes time and the old drug susceptibility testing methods can only identify this mutant bacteria when it is in more than 1% of the bacteria. But, with this novel targeted deep sequencing method the scientists could identify the mutant bacterium when it is present in only 0.1% of all the TB bacteria in the patient’s body. This means they can detect resistance quicker than the older methods.
The usual “gold standard” way of testing for resistance is to grow the patient’s TB bacteria in a laboratory in a medium that contains the antibiotic that needs to be tested.
If the bacteria grow in the presence of the drug, it means that it is resistant to the drug. If it doesn’t grow, it means that it is susceptible and the patient can still be treated with that drug.
But this method is slow because the bacterium grows very slowly. It can take up to eight weeks to get a result. This does not benefit the patient, because in that time the bacterium may gain resistance to other drugs.
The researchers argue that their results show that it is crucial to monitor patients receiving bedaquiline and to develop new diagnostic tools to rapidly identify resistance.
The aim is to minimise resistance as much as possible. Each patient should be treated with at least five drugs that “we know will be effective against the particular TB bacteria that are causing disease for that patient.”
The method used in this study is expensive and is not routinely available to TB patients. But it may inspire or be the basis for developing more affordable ways to test for resistance.