22 May 2020
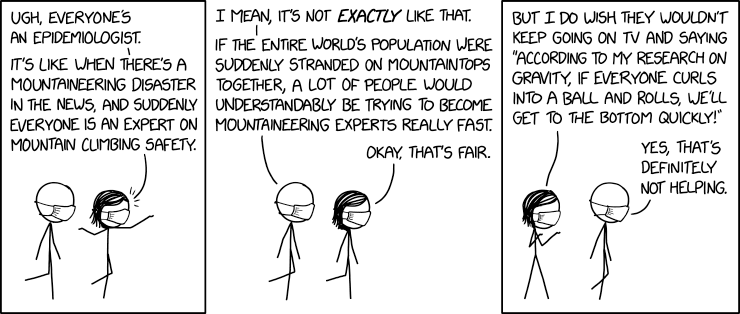
Many models of the unfolding Covid-19 pandemic in South Africa have been presented. Cartoon by xkcd (Creative Commons Attribution-NonCommercial 2.5 License)
A week ago many were complaining about the lack of published models by government to explain Covid-19 decision-making. On Thursday the Department of Health hosted a Zoom call in which more models were presented than could fit on a Milan catwalk.
Some models are useful. If modellers carefully explain their assumptions and present multiple scenarios, we can get a better understanding of the epidemic’s possible trajectories, or the potential of different interventions to reduce the number of infections.
But models, especially because they are surrounded by fancy equations, can give a false sense of certainty. No one truly knows how the epidemic will play out. We humans, in contrast to any other species, have an insatiable desire to know the future. But we can’t. We can only make educated guesses based on the limited information at our disposal, and when it comes to Covid-19 that information is still very limited indeed.
Some common uncertainties that stand out in the models are the rate of asymptomatic infections, how infectious SARS-CoV-2 is, how effective various interventions are, and the death rate.
A number of the models suggest that South Africa will not have enough ICU beds for everyone who will need one. Estimates of Covid-19 deaths range from a few thousands to several hundreds of thousands.
Here then is a very brief summary of each model and a link to more information about it.
The South African Covid-19 Modelling Consortium mainly consists of researchers from the universities of Cape Town, Stellenbosch, Wits and the National Institute of Communicable Diseases (NICD). It is the main model that the health department is using.
The model makes projections under optimistic and pessimistic scenarios with epidemic peaks in August and July, respectively. It projects six months into the future.
Under the two scenarios this model estimates between 34,000 and 50,000 deaths by November, although the modellers stress the significant uncertainty about these numbers. “These projections are subject to considerable uncertainty and variability. Estimates will change and improve as the epidemic progresses and new data become available.”
The model assumes that after the lifting of hard lockdown measures, level four remains in place for one month, and after that social distancing measures reduce transmission by 10 to 20%.
Even in the optimistic scenario ICU capacity is exceeded by many thousands of beds in August to September. While they do not factor in the additional deaths that this will cause, it might be considerable given that ICU bed capacity is about 3,300 and that the need for ICU beds may exceed 20,000 to 30,000 at the peak of the epidemic.
The modellers estimate that dealing with Covid-19 will require R26 to R32 billion over the next six months, of which R10 to R15 billion will accrue to the national health department. (South Africa’s health budget for this year is about R230 billion, and the national department has allocated R20 billion to Covid-19.)
(Note that government originally was using a very simple, but possibly no less prescient, model developed by some of the members of this consortium, that we described here.)
On 29 April the Actuarial Society of South Africa warned that as many as 48,000 people may die of Covid-19 in the following four months if “government does not maintain a strict approach to flattening the curve”. The society also projected that the need for ICU beds may peak at 10,000, significantly above the estimated 3,300 capacity. The society is open about the very significant uncertainty in its model and has indicated that it is being updated, with new projections to be shared soon. (This Powerpoint presentation of the ASSA model, dated 21 May, may indeed be an update, but we’re struggling to read the graphs.)
A model by Alex van Den Heever of the Wits School of Governance looks at strategies for keeping the epidemic suppressed, or, to put it technically, to get R below 1 (see this explanation of R). His model is not concerned with trying to predict the future. Some of the interventions he considers are testing and contact tracing, lockdown, closing borders, social distancing and workplace protocols. He also considers the effect of cold and warm weather (other coronaviruses transmit a bit less efficiently in warm weather so this is a reasonable assumption for SARS-CoV-2).
Van den Heever has argued that if government is using a strategy that assumes R goes above 1 (like the one we described above), then it has effectively given up, because the epidemic will run out of control. His model on the other hand envisages the switching off and on of a selection of interventions as the epidemic is suppressed here and resurges there. Vital to this strategy is good contact tracing, but Van den Heever has expressed frustration at the poor quality of government’s test and trace strategy so far.
Van den Heever has described his model in detail here.
Most of the models of the epidemic are what’s called compartmental ones; they divide the population into compartments (susceptible, exposed, infectious, recovered, and so on) and then describe how people move between these compartments with a set of equations.
A different kind of model is the SABCoM one developed by researchers at UCT. This simulates how people move around and transmit or contract Covid-19. The creators of this model deserve credit for making the computer code of their model available online. They have applied their model to each ward in Cape Town, but, as with the Van den Heever model, rather than predicting the future, their main aim appears to be to see what the effect of different interventions are on the epidemic.
Alternatives to lockdown exist, they write, but must be done properly. In particular they emphasise the importance of effective contact tracing.
Auditing and consulting firm Deloitte has developed a model for Business for South Africa (B4SA) to assist B4SA in its engagement with government. The model projects the need for hospital beds, oxygen, ventilators, N95 masks etcetera.
The London School of Hygiene and Tropical Medicine has produced a model of the South African epidemic that estimates 310,000 deaths if there are no interventions (more than died of AIDS in South Africa in 2005, the worst year of the HIV epidemic). Introducing social distancing as well as “shielding” high-risk people from infection, can reduce the number of deaths considerably, to below 100,000 if implemented very effectively. Charles Simkins explains the model well on Politicsweb.
A group called Pandemic Data Analysis estimates only 20,000 deaths with, as they write, “a sense that we might bring it down or decide that it is the top of our range.”
Researchers at the University of East Anglia have used Chinese and Italian data to estimate the number of deaths in many countries for different infection rates, corrected for age distribution, including South Africa. We’ve previously explained their work.